About dystrophic epidermolysis bullosa (DEB)
DEB is a type of epidermolysis bullosa (EB) that is a serious genetic disease1,2
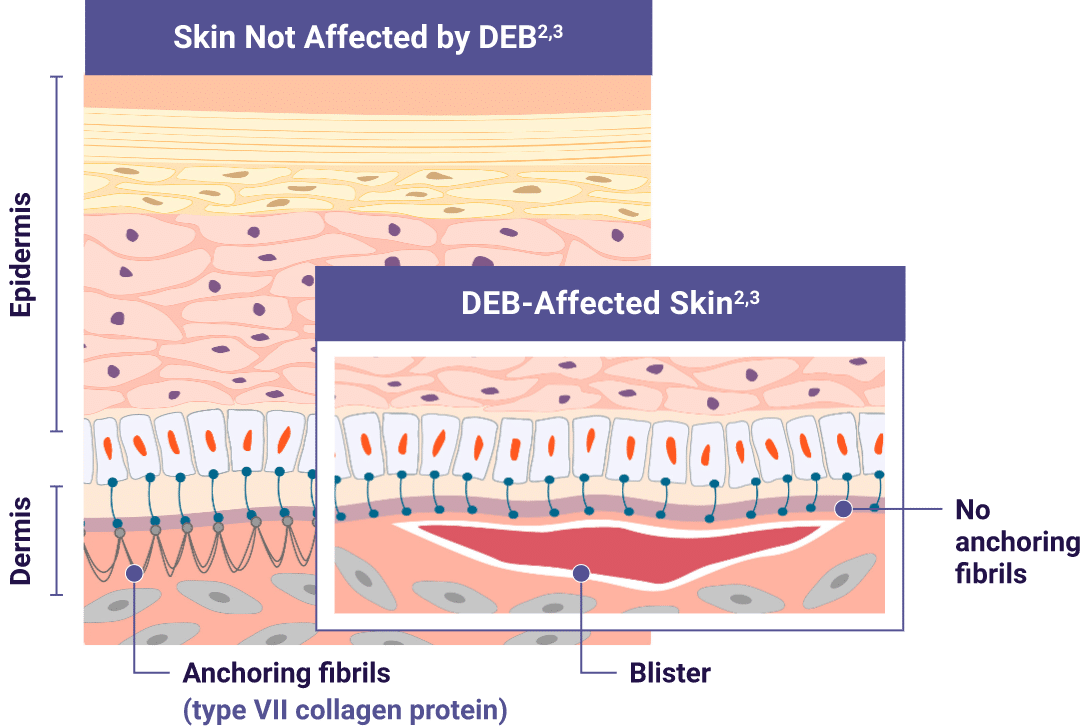
Adapted from De Rosa L, Latella MC, Secone Seconetti A, et al.
Cold Spring Harb Perspect Biol. 2020.
- DEB is caused by mutations in the COL7A1 gene, resulting in the lack of functional type VII collagen, which disrupts the formation of anchoring fibrils in the skin and prevents adhesion of the epidermis to the dermis1
- There are 2 types of DEB based on inheritance patterns: dominant (DDEB) and recessive (RDEB)1
- Regardless of type, patients and families can face significant physical, emotional, and financial burdens1
Genetic testing can confirm a DEB diagnosis.1,4,5
Learn more about genetic testing for DEB.
DEB can lead to serious symptoms and complications4
DEB symptoms primarily include skin fragility, blistering, and wounds, and can also result in damage to the mucosa and epithelial lining of organs4
Patients with DEB require active and vigilant surveillance for serious complications.
Some serious complications include1,4,6:
- Infection of open wounds
- Esophageal stricture
- Gastrointestinal and genitourinary issues
- Cutaneous squamous cell carcinoma (SCC)
DEB wounds can increase the risk of developing cutaneous SCC, regardless of genetic subtype (RDEB or DDEB), size, or chronicity—so proactively managing all DEB wounds is critically important to the health and well-being of patients.7
Learn about a treatment option
See How It WorksVYJUVEK is a topical gel indicated for the treatment of wounds in patients 6 months of age and older with dystrophic epidermolysis bullosa (DEB) with mutation(s) in the collagen type VII (COL7A1) gene.
WARNINGS AND PRECAUTIONS
Accidental Exposure to VYJUVEK gel: VYJUVEK will not replicate in the subject’s cells and does not integrate into the subject cells’ native genetic material. For precautions, avoid direct contact with treated wounds (e.g., touching or scratching) and dressings of treated wounds for approximately 24 hours following treatment. Wear protective gloves when assisting subjects with changing wound dressings and handling the disposal. In the event of accidental exposure (e.g., through a splash to the eyes or mucous membranes), flush with clean water for at least 15 minutes.
Clean all surfaces that may have come in contact with VYJUVEK biological suspension or gel and treat all spills with a virucidal agent.
Dispose all materials (e.g., vial, syringe, needle, cleaning materials) that may have come in contact with VYJUVEK biological suspension or gel into a biohazard bag or container.
ADVERSE REACTIONSThe most common adverse reactions (>5%) were itching, chills, redness, rash, cough, and runny nose.
- Please see Important Safety Information above and click here for full Prescribing Information.
1. Denyer J, Pillay E, Clapham J, eds. Best Practice Guidelines: Skin and Wound Care in Epidermolysis Bullosa. Wounds International; 2017.
2. Eichstadt S, Barriga M, Ponakala A, et al. JCI Insight. 2019;4(19):e130554. doi:10.1172/jci.insight.130554
3. De Rosa L, Latella MC, Secone Seconetti A, et al. Cold Spring Harb Perspect Biol. 2020;12(5):a035667 5.
4. Bardhan A, Bruckner-Tuderman L, Chapple ILC, et al. Epidermolysis bullosa. Nat Rev Dis Prim. 2020;6:78.
5. Has C, Bauer JW, Bodemer C, et al. Consensus reclassification of inherited epidermolysis bullosa and other disorders with skin fragility. Br J Dermatol. 2020;183:603.
6. Bruckner AI, Losow M, Wisk J, et al. The challenges of living with and managing epidermolysis bullosa: insights from patients and caregivers. Orphanet J Rare Dis. 2020;15:1.
7. Condorelli AG, Dellambra E, Logli E, Zambruno G, Castiglia D. Epidermolysis bullosa-associated squamous cell carcinoma: from pathogenesis to therapeutic perspectives. Int J Mol Sci. 2019;20(22):5707.
VYJUVEK is a topical gel indicated for the treatment of wounds in patients 6 months of age and older with dystrophic epidermolysis bullosa (DEB) with mutation(s) in the collagen type VII (COL7A1) gene.
WARNINGS AND PRECAUTIONS
Accidental Exposure to VYJUVEK gel: VYJUVEK will not replicate in the subject’s cells and does not integrate into the subject cells’ native genetic material. For precautions, avoid direct contact with treated wounds (e.g., touching or scratching) and dressings of treated wounds for approximately 24 hours following treatment. Wear protective gloves when assisting subjects with changing wound dressings and handling the disposal. In the event of accidental exposure (e.g., through a splash to the eyes or mucous membranes), flush with clean water for at least 15 minutes.
Clean all surfaces that may have come in contact with VYJUVEK biological suspension or gel and treat all spills with a virucidal agent.
Dispose all materials (e.g., vial, syringe, needle, cleaning materials) that may have come in contact with VYJUVEK biological suspension or gel into a biohazard bag or container.
ADVERSE REACTIONSThe most common adverse reactions (>5%) were itching, chills, redness, rash, cough, and runny nose.
- Please see Important Safety Information above and click here for full Prescribing Information.
1. Denyer J, Pillay E, Clapham J, eds. Best Practice Guidelines: Skin and Wound Care in Epidermolysis Bullosa. Wounds International; 2017.
2. Eichstadt S, Barriga M, Ponakala A, et al. JCI Insight. 2019;4(19):e130554. doi:10.1172/jci.insight.130554
3. De Rosa L, Latella MC, Secone Seconetti A, et al. Cold Spring Harb Perspect Biol. 2020;12(5):a035667 5.
4. Bardhan A, Bruckner-Tuderman L, Chapple ILC, et al. Epidermolysis bullosa. Nat Rev Dis Prim. 2020;6:78.
5. Has C, Bauer JW, Bodemer C, et al. Consensus reclassification of inherited epidermolysis bullosa and other disorders with skin fragility. Br J Dermatol. 2020;183:603.
6. Bruckner AI, Losow M, Wisk J, et al. The challenges of living with and managing epidermolysis bullosa: insights from patients and caregivers. Orphanet J Rare Dis. 2020;15:1.
7. Condorelli AG, Dellambra E, Logli E, Zambruno G, Castiglia D. Epidermolysis bullosa-associated squamous cell carcinoma: from pathogenesis to therapeutic perspectives. Int J Mol Sci. 2019;20(22):5707.
For US Healthcare Professionals Only
This website is intended for US healthcare professionals.
Would you like to continue?
